During the past six years, the Department of Health and Human Services Office of the Inspector General (OIG) has made at least five reports regarding improper or questionable billing for sleep studies or polysomnography (PSG). In a recent report regarding polysomnography billing, the OIG found, among other items, that some providers’ documentation was incomplete and some attending technicians or technologists lacked the required credentials or training certifications.
What Is Polysomnography?
Part B of the Medicare program includes supplementary medical insurance for PSG services and associated medical supplies.
Medicare coverage for polysomnography services includes a diagnostic sleep study and, depending on a beneficiary’s diagnosis, may also include a positive airway pressure (PAP) titration study. Providers conduct a diagnostic sleep study to diagnose medical conditions that can affect sleep, most commonly obstructive sleep apnea (OSA), and to evaluate how effectively PAP devices manage the beneficiary’s condition. If the study indicates that a patient has a sleep disorder, then the provider may conduct a PAP titration study.
Providers normally perform PSG services at sleep disorder clinics, which may be either affiliated with hospitals or be freestanding facilities, such as independent diagnostic facilities or provider-owned laboratories.
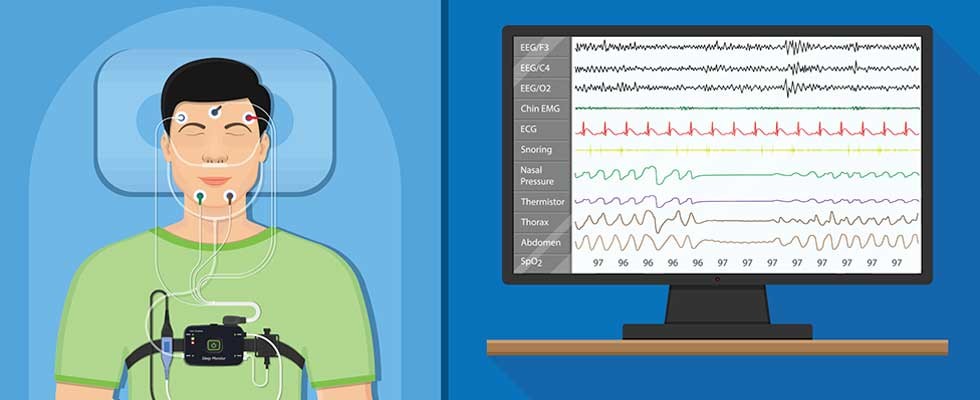
For the test, a beneficiary sleeps overnight while connected to sensors that measure and record sleep parameters such as brain wave activity, eye movement and air flow. If PSG shows that a beneficiary has sleep apnea, a provider may prescribe a PAP device for treatment. Providers fit and titrate PAP devices (i.e., set them to the appropriate pressure for the user), after which beneficiaries may receive a PAP device for home use. Providers also may prescribe a different type of treatment device, called an oral appliance, instead.
Providers can perform diagnostic and titration services in two visits or together in a single visit, known as a split-night service. Providers can perform a split-night service when a diagnosis of sleep apnea can be made within the first few hours of the polysomnography service and the provider is able to fit and titrate the PAP device in the same night. If the provider cannot make a diagnosis early in the sleep test, the beneficiary may need to return later for an additional PSG service to fit and titrate the PAP device.
How Medicare Pays
Medicare pays for sleep tests under the Medicare Physician Fee Schedule when performed in freestanding facilities and under the Outpatient Prospective Payment System when performed in a hospital outpatient department. Providers must use standardized codes, called Current Procedural Terminology codes, to identify the service.
All PSG services consist of two components: the administration of the test, which is the technical component, and the provider’s interpretation of the test, which is the professional component. Providers use modifier code -TC or -26, respectively, to indicate whether the billing is for the technical or professional component. If a provider does not include a modifier code on the claim, it indicates that the provider
is billing for a “global service.” A provider that bills for a global service receives payment for both the technical and professional components.
Medicare covers all reasonable and necessary diagnostic tests given for sleep disorders only if the patient has symptoms such as:
Narcolepsy, a syndrome characterized by abnormal sleep tendencies, such as excessive daytime sleepiness or disturbed nocturnal sleep
- OSA, a potentially lethal condition in which the patient stops breathing during sleep
- Impotence, as shown by diagnostic nocturnal penile tumescence testing, which may be covered under limited circumstances, to see whether erectile impotence is organic or psychogenic
- Parasomnias, a group of conditions that represent undesirable or unpleasant occurrences during sleep
From the OIG
In a recent report regarding PSG billing, the OIG found two major issues:
1.Some Providers’ Medical Record Documentation Was Incomplete
Medicare will cover all reasonable and necessary diagnostic testing for sleep disorders only if the patient has symptoms such as those listed above and all of the following criteria are met:
- the clinic is either affiliated with a hospital or is under the direction and control of physicians;
- patients are referred to the sleep disorder clinic by their attending physician and the clinic maintains a record of the attending physician’s orders; and
- medical evidence confirms the need for diagnostic testing, such as physician examinations and laboratory tests.
Furthermore, most local coverage determinations (LCDs) published by Medicare Administrative Contractors for sleep testing specify that providers must maintain a record of the attending physician’s order and the medical record documentation supporting the medical necessity of services performed. This documentation includes, but is not limited to, a face-to-face evaluation by the treating physician that documents relevant medical history and symptoms, a physical examination and the results of pertinent diagnostic tests or procedures.
In its recent report, the OIG found that certain providers’ documentation was incomplete because it did not contain the face-to-face clinical evaluation, the physician’s order or the technician’s report.
2. Some Attending Technicians or Technologists Lacked the Required Credentials or Training Certifications
Some LCDs state that sleep technicians or technologists who attend PSG services must have appropriate training certifications, such as Registered Polysomnography Technologist or Registered Electroencephalographic Technologist.
The OIG found that some providers billed for a polysomnography service but the attending technologists’ credentials or training certifications had expired or the provider did not properly document the credentials or certification.
If you have any questions about billing for polysomnography services, you should consult with your health care attorney.
